COUNTERPOINT: Why Medicaid reform is appropriate
Published in Op Eds
Battle lines are being drawn in Washington over whether to reduce spending on Medicaid and the Children’s Health Insurance Program (CHIP). The debate, however, should not be framed solely as a fight over cuts. It should focus on reform. There is a need and an opportunity to rein in Medicaid and CHIP costs without compromising the safety net for those who are in need.
From Fiscal Year 2019 to Fiscal Year 2024, federal spending on these programs surged from $409 billion to $626 billion, representing a 53 percent increase. During that period, inflation and population growth combined to total 28%. In addition, improper payments under Medicaid and CHIP were estimated at $32 billion in 2024. No private-sector organization would sustain that amount of increase and level of waste without acting.
Taxpayers deserve greater accountability, and vulnerable Americans require a stable safety net. Reform does not mean abandonment. It means modernization, targeting, responsibility and accountability. There are several practical steps that Congress should take now to address the issues before it is too late.
First, enact and enforce work requirements for able-bodied adults without dependent children. Medicaid and similar programs must serve as springboards to independence, not long-term crutches. Requiring work, job training, or community engagement restores accountability, fosters personal responsibility, and reinforces the dignity that comes with self-sufficiency.
Second, terminate the remaining COVID-era expansions of Medicaid and CHIP. The public health emergency has long since ended. It is time to roll back the extraordinary measures that were meant to be temporary. Allowing them to linger drives up costs and dilutes the focus of these programs, preventing them from helping those in need.
Third, restrict federal Medicaid funding to documented residents only. Emergency services for undocumented immigrants may remain, but such coverage should be the responsibility of states that choose to provide it — without federal reimbursement. Continuing to subsidize such coverage invites further undocumented immigration and undermines enforcement efforts.
Fourth, crack down on state-level reimbursement schemes that exploit loopholes to game the federal match system. These practices siphon taxpayer dollars and distort the original purpose. Federal authorities must strengthen oversight and impose penalties to end these backdoor budget gimmicks and system abuses.
Fifth, tighten federal oversight by enhancing audits, upgrading internal controls, and ramping up enforcement. Fraud, waste and abuse must be aggressively rooted out. While some level of error is inevitable in large systems, tolerance for it should never be. Every misallocated dollar is a missed opportunity to support someone who genuinely needs help.
Finally, lawmakers should consider capping federal costs and providing states more flexibility through block grants with minimal federal standards. States understand their populations better and can design more efficient, effective programs as long as accountability remains in place.
Of course, reforming Medicaid and CHIP is just one piece of a larger puzzle. The broader U.S. healthcare system is unsustainable. Healthcare costs are the second-largest driver of future federal spending, behind only interest on the debt. And despite spending more of our economy on healthcare than any other nation, our outcomes are below average for an industrialized nation. That is unacceptable.
We must move away from the fee-for-service model, which rewards volume over value. Instead, payments based on capitation and diagnosis payment approaches can promote better care at a lower cost. Prescription drug policy also requires reform, including expanded price negotiations, shared research and development responsibilities, and a ban on direct-to-consumer advertising.
Liability reform is also long overdue. Adopting safe-harbor standards of care would curb unnecessary services and reduce malpractice litigation costs. In addition, the federal government should implement recommendations from the Institute of Medicine’s 2014 End of Life study, which I co-chaired. These proposals offer practical, cost-effective improvements for Medicare and other federal programs.
We must also make subsidies and premiums more progressive. Healthcare financial aid should be more progressive. Additionally, the tax exclusion for employer-provided health insurance should be scaled back. It disproportionately benefits higher-income households and those with more generous healthcare plans while distorting insurance markets.
In the long term, we must reconsider the federal role in healthcare. One option is a universal, publicly funded plan that covers preventive, wellness and catastrophic care. Americans could purchase supplemental coverage, while additional federal efforts would focus on veterans, low-income individuals and those with disabilities.
It is time to face the facts. Medicaid and CHIP have grown dramatically, are inefficient and vulnerable to abuse. Reform is not only responsible but also essential. Delaying action puts taxpayers and those in need at risk. Our public health and fiscal future depend on getting this right.
_____
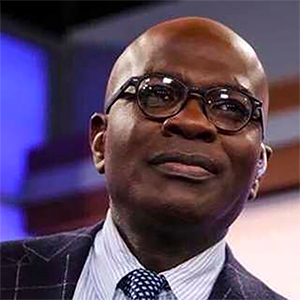
ABOUT THE WRITER
David M. Walker is the former comptroller general of the United States. He wrote this for InsideSources.com.
_____
©2025 Tribune Content Agency, LLC






















































Comments